Pavilion Publishing and Media Ltd
Blue Sky Offices Shoreham, 25 Cecil Pashley Way, Shoreham-by-Sea, West Sussex, BN43 5FF, UNITED KINGDOM
Sexual dysfunction in young men: Part 2
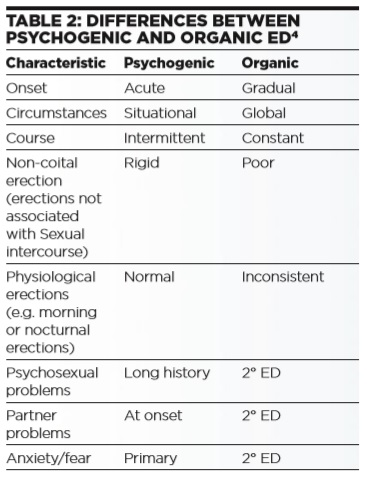
In the second part of our series on sexual dysfunction, the authors look at erectile dysfunction, Peyronie’s disease and hypoactive desire disorder.
---------------------------
This content is restricted to members of Pavilion Health Today. If you are an existing user, please log in. New users may register for free below.